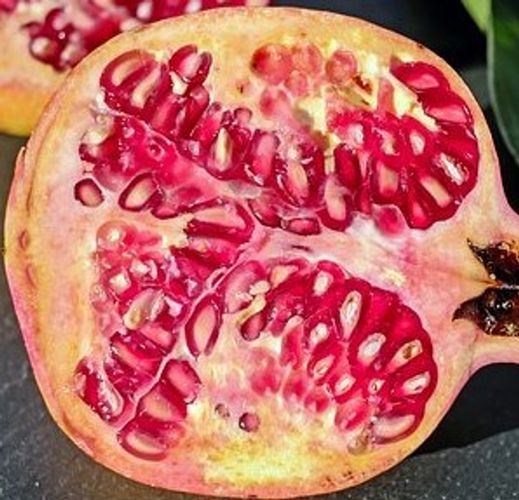
(Yes, this is a pomegranate, somewhat similar to but easier to look at than, a polycystic ovary).
10% of all women of child-bearing age have it, along with 75% of women with irregular periods, and it is the most common cause of female-associated problems with infertility. So if you have been diagnosed with it, you have lots of company.
Polycystic ovarian syndrome, or PCOS, usually begins around the time of first menstruation, but it can also start much later in a woman’s life. And there is often a long delay before it is even suspected or diagnosed. The most important thing about PCOS to remember, however, is that it is a condition involving the entire endocrine system: despite the name, PCOS not just about the ovaries.
PCOS signs and symptoms
What might cause you to suspect you could have PCOS?
- Irregular periods or long spans with no period without ovulation, and perhaps having started your period very early (before 10 years old)
- Male hormone dominance (androgen hormones)
- Male hair pattern, called “hirsutism” (basically, hair in places you don’t want it as well as hair loss at the crown of your head consistent with male pattern baldness)
- Acne (usually along the jaw line, rather than the more typical “T-zone”)
- Infertility or recurring miscarriages
- Obesity
- Type 2 diabetes
- Sleep apnea
- Metabolic Syndrome (a combination of high blood pressure, high cholesterol, type 2 diabetes and large waist circumference)
Notice that many of these lead to separate diagnoses, so it’s the combination that matters. Interestingly, while PCOS typically involves enlarged ovaries with multiple cysts that can be detected by a physical exam (usually confirmed by an ultrasound), it is possible to be diagnosed with it even if you don’t have ovarian cysts. It’s also possible to have ovarian cysts and NOT have PCOS.
What is known about PCOS is that it involves problems with management of insulin (the “mother” endocrine hormone), male hormone dominance, low-grade inflammation and often runs in the female family line. If not addressed, PCOS usually progresses gradually through a woman’s lifecycle, including after menopause, which means that without intervention many symptoms tend to worsen with time[i].
Is it PCOS?
It takes an average of 2 years and 3 doctors to get a diagnosis, and this does not include the years before it’s even suspected.
PCOS involves multiple symptoms, but the ovarian cysts themselves can be confused with endometriomas (sometimes called “chocolate cysts”), which are tissue growths appearing in the ovaries for 20-40% of women who are in an advanced stage of endometriosis, a different condition. The best way to confirm that the cysts are due to PCOS and not endometriosis is with an ultrasound.
And there are other rabbit holes. Irregular periods that are characteristic of PCOS can be caused by other conditions: adrenal or ovarian tumors, thyroid problems, congenital adrenal hyperplasia (a problem of functioning of the adrenal glands, which sit on top of the kidneys), hyperprolactinemia (overproduction of the hormone prolactin), acromegaly (a condition involving excess production of growth hormone) and Cushing syndrome (resulting from high levels of the hormone cortisol).
A diagnosis of PCOS usually involves ruling out these conditions, which is why the process often takes years. Along the way are a number of lab tests such as an endocrine panel (including a test for androgens, or male hormones), blood sugar and cholesterol, and imaging tests (ultrasonography, CT scan or MRI).
Conventional treatment[ii]
Initial conventional treatment of PCOS is actually something that most integrative practitioners might also recommend: lose at least 5% of body weight. Along with weight loss, exercise is often recommended.
Conventional drug treatment offered for PCOS usually primarily addresses the specific symptoms that are associated with it, such as blood pressure, type 2 diabetes, acne or cholesterol. For younger girls experiencing irregular periods, oral contraceptives might be recommended. Women having problems conceiving are often prescribed Clomid, a hormonal fertility drug.
Surgery for PCOS (called “laporoscopic ovarian drilling”) is occasionally recommended, which involves removing parts of the ovary. For women trying to conceive, this usually increases the chances of getting pregnant. But like any surgery, the procedure comes with risks.
What you can do on your own
Some women do not experience PCOS symptoms until they have gained a lot of weight, which unmasks the underlying condition. This is the reason why weight loss can have a significant positive impact on the health of women with PCOS.
Along with weight loss, women with PCOS can take other steps on their own to help balance their endocrine system, such as eating whole foods, plenty of healthy fats (such as coconut and olive oil), and avoiding foods, chemicals and other substances and many household and personal care products that are endocrine disruptors (make sure you read labels!).
Adequate daily exposure to sunlight also helps feed the endocrine system. I usually suggest about 30 minutes of daily sunlight exposure without sunscreen or sunglasses. Of course, during the summer months, this needs to be timed carefully in order to avoid sun damage or heatstroke!
How I address PCOS
If you decide to choose natural remedies for your PCOS, I will conduct a detailed assessment of your symptoms: when they started and how they have progressed since then. I will also try to find out as much as possible about who you are as a person. This is because I am a holistic health care practitioner.
Because PCOS is a complex hormonal system condition, addressing it requires a multi-pronged approach involving a series of steps[iii], as well as something else: patience. Homeopathic care to resolve the underlying processes that cause PCOS is several months and often longer.
I already mentioned weight loss and lifestyle changes, which are firstline interventions, also recommended by conventional health care practitioners. If weight loss is a first step that has been recommended for you, please call or Email and ask me about metabolic balance®, the personalized nutrition program I am certified to coach that can help you achieve weight loss and long-term weight management by balancing your metabolism using only whole foods.
If Type2 diabetes is also part of the metabolic picture, there are specific homeopathic medicines that can help restore a balanced sugar metabolism.
Sometimes, adverse effects of previous drug treatments, surgery or other “hormonal insults” need to be addressed early on.
Other homeopathic remedies can be used to strengthen specific organs or systems. With PCOS, there is frequently thyroid, liver and cardiovascular involvement.
As important as systemic approaches are, they may not be sufficient for many women. This is because certain PCOS symptoms can be extremely distressing and disruptive.
For example, multiple cysts in the ovaries or irregular periods can be associated with severe intermittent pain, which can be addressed homeopathically.
Hirsutism (i.e. hair in places you don’t want) and acne are other PCOS symptoms very concerning to many girls and women. Fortunately, homeopathy can help reduce these as well.
For more information, visit my profile, follow me, and learn about WellnessCareOnline, which focuses on balancing hormones, metabolism, weight and mood. And call me for a free 15-minute consultation to learn more about how I work with clients.
What have you done that has helped your PCOS symptoms?
[i] Hari, S, “What causes PCOS and how will it affect my body?”: https://www.endocrineweb.com/conditions/polycystic-ovary-syndrome-pcos/what-causes-pcos-how-will-it-affect-body
[ii] https://emedicine.medscape.com/article/256806-overview
[iii] Thanks to Karen Allen CCH for her years of work helping women with PCOS and other endocrine issues, and for much of the information in this section.