The Journey of Digestion – Part 3
In the first two blogs on Digestion, we learned the importance of chewing our food, and what happens when the food (bolus) leaves our mouth and travels down through the esophagus to our stomach, where our food (chyme) is digested even further by our digestive enzymes. For some, digestive difficulties begin at this phase of digestion – hiatal hernias, GERD, gastritis, etc. If you’re having difficulty at this phase, please (re)read Part 2 for natural ways to improve your gut health.
So what happens now to this chyme as it continues its journey of digestion? Well, from the stomach it passes through our pyloric sphincter, into the small intestine (which isn’t so small at about 20 feet). The small intestine is made up of three distinct parts: duodenum, jejunum, ileum – each part has its own role in our digestion.
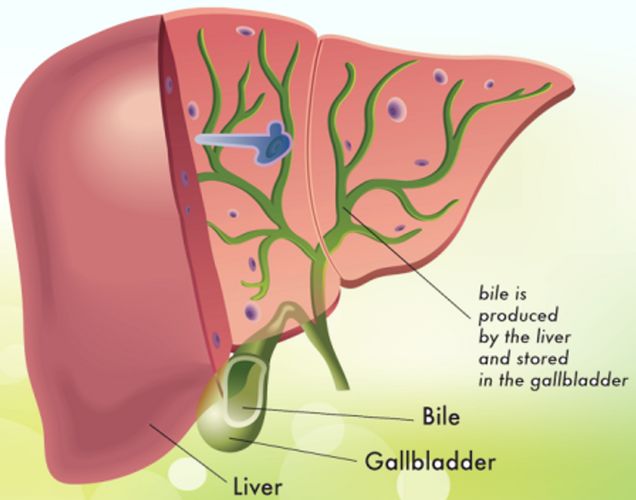
The first part (duodenum) introduces pancreatic enzymes and bile from the gallbladder to begin to chemically breakdown and digest fats (into water soluble substance that can be transported into our bloodstream). The big question always arises, as I know I asked – what happens if I don’t have a gallbladder? While there is no absolute, as everyone is different, there are some things that can be done if you are having difficulty digesting fats.
Before getting into that, let’s talk a little about the gallbladder and why it is removed in the first place. Basically the gallbladder is a holding tank for bile. Metaphorically (hypnotherapists love metaphors), bile is like a detergent that dissolves the grease (fats) in the chyme. When too much bile is built up in the gallbladder, gallstones begin to form. Gallstones are formed when a diet is too high in fat or oxidized oils (i.e., excessive use of olive oil at high heat where it is being oxidized); allergies to dairy and eggs; low stomach acid; too little fiber; and chronic stress to name a few.
Surprisingly, the removal of the gallbladder (cholecystectomy) is the most frequently performed surgery in the U.S., with over half a million gallbladders removed each year. And the gallbladder isn’t even responsible for the stones – the liver is.
So if you’re like me (and a few of my family members), you’ve had your gallbladder removed and now what? Well, we actually trade one problem in for other ones – our liver becomes more compromised; bile is continually dumping a minimal amount into the intestinal tract, which can lead not only to digestive disturbances, but also nutritional deficiencies (absorption of vitamins A, D, E, K, and essential fatty acids is very likely to be impaired). Another metaphor on how the bile is now released: It’s like a leaky faucet that drips constantly, but that you can never get to turn on full blast when you need to.
Back to what can be done – bile salts – bile in tablet form (ox bile supports the body in breaking down fats without the presence of bile). Personally I use Standard Process Laboratories’ Cholacol at every meal that I consume fats and oils. (Keep in mind that I am not a doctor and that this is simply what I DO.) Other natural supplements that will help include:
- Choline - an important nutrient following a cholecystectomy as it helps support the natural digestion of dietary fats and can work well in combination with bile salts to help prevent excessive gas and bloating.
- Betaine - another nutrient that helps our body breakdown and absorb fats. This nutrient helps maintain our metabolism and also limits some of the side effects, such as bloating, gas, and diarrhea, following surgery. Betaine is naturally found in beets, or supplementally in capsule or powder form.
- Lecithin - an additional supplement that supports digestive function following gallbladder removal. Research suggests that this substance keeps cholesterol from solidifying in our body and helps support our digestion of fats. It is found in foods such as oatmeal, eggs, and peanuts; or in the form of a supplement or powder (soy or sunflower).
Something that was mentioned in an earlier blog also applies here: cleansing your liver using lemon juice or drinking diluted apple cider vinegar. My daily drink is 1 tablespoon ACV (Braggs), 2 tablespoons lemon juice, local honey (for sweetness & probiotics) and a dash of MCT (medium chain triglyceride) oil in 6-8 ounces of water. MCTs do not rely on the production of bile to be metabolized and begin breaking down immediately from contact with enzymes found in saliva.
Studies show that people who have been through a cholecystectomy, with or without gallstones, run a greater risk of developing SIBO (small intestinal bacterial overgrowth) over time (4-6 months shows no increase in SIBO, but 2 to 12 years is statistically proven that there is increased incidence of SIBO).
At this point in our discussion, we are at the very first part of our small intestine – remember that 20-foot tube? Once we leave the duodenum, it’s on to the jejunum and ileum.
The jejunum has a lining that is specialized in the absorption of carbs and proteins, which is the uptake of nutrients into the system. The proteins were broken down in the stomach, and the carbohydrates are further broken down in the duodenum by enzymes from the pancreas and the liver, into simple sugars. These are the sugars that feed our cells for the creation of energy.
The last section of the small intestine is the ileum, whose main function is to absorb vitamin B-12 and whatever products of digestion that were not absorbed by the jejunum.
From here, all waste products are moved out of the small intestine into our colon (large intestine). The large intestine needs to reabsorb water and electrolytes from the remaining products into our bloodstream. The indigestible waste products then move through the rectum and anus in the form of poop.
Our Digestive Journey continues in our next blog, as we return to the colon and the liver.
Until then,
To Your Health & Happiness,
Michele Root ~ Empowering You!