Gut-Brain-Axis (GBA)
We’ve covered a lot of ground in the past with blogs on Stress and the long & winding road of our Digestive system. I want to intertwine what we have discussed and speak on the Gut-Brain connection to see the correlation.
It’s been said that we have a second brain – in our gut. This second brain is just as powerful our “central” brain. Like Siamese twins, these two brains are interconnected; when one gets upset, the other does too. Nearly every substance that helps run and control the brain has turned up in the gut. Our gut contains 100 million neurons – more than the spinal cord.
The origin of the GBA takes place early, during the prenatal period, directly after the beginning of neurodevelopment. A key role in the formation of the brain.
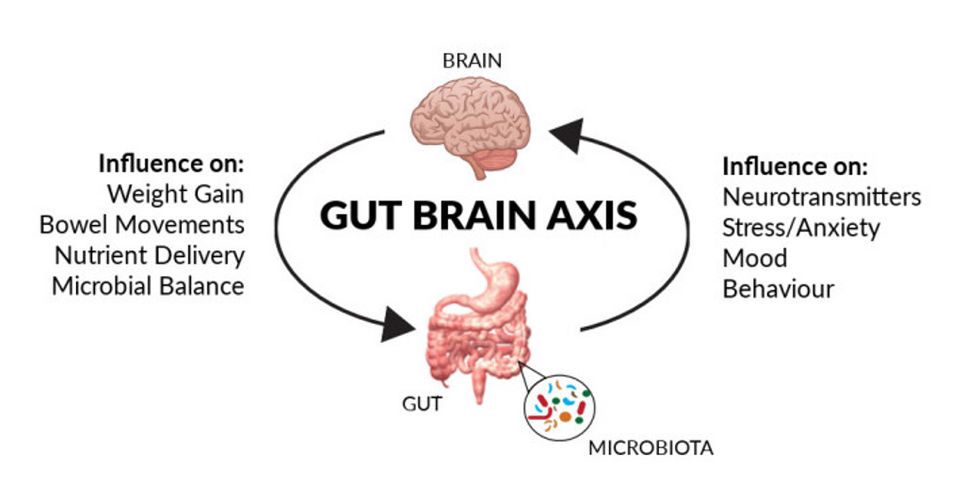
So how do these two brains communicate? A superhighway of sorts ~ a bi-directional pathway where neurotransmitters and hormones are sent back and forth along the GBA. It happens not only through nerve connection between the organs, but also through biochemical signals such as hormones that circulate in the body. This superhighway links our emotional and cognitive centers (central nervous system, autonomic nervous system, enteric nervous system) with our peripheral intestinal functions (immune activation, intestinal permeability [aka leaky gut]). It primarily combines the sympathetic and parasympathetic “arms” of the autonomic nervous system, which drives neural signals between the gut and brain.
Our autonomic nervous system (ANS) is responsible for controlling our bodily functions not consciously directed, such as breathing, heartbeat, and digestive processes. It is divided into two parts: Sympathetic (prepares the body to run away from threat [fight, flight or freeze] by stimulation of blood flow to major muscles and restricting gut motility) and the parasympathetic (controls digestion & relaxation [rest & digest] that conserves energy, slows heart rate).
Our enteric nervous system (ENS) is embedded in the lining of the gastrointestinal [GI] system consisting of our esophagus, stomach, small intestine and colon. It is considered a single entity and contains millions of neurons that can respond to neurotransmitters and send signals up to the brain.
Intestinal permeability refers to the physical gaps between intestinal cells, which is thought to be partly regulated by the microbiome. Leaky gut was coined to describe when those gaps are enlarged and external substances & waste products are allowed to pass into the bloodstream. This has been associated with mood changes, immune function and inflammation. Leaky gut may be associated with numerous conditions like IBD, autoimmune conditions such as Type I diabetes and Celiac.
The superhighway is our Vagus nerve – our tenth cranial nerve, and the largest in our body, that wanders from our brainstem to our intestines. It’s the prime driving force of the parasympathetic nervous system which, as discussed, regulates our rest/digest (tend/befriend) responses.
When the central brain encounters a frightening situation, it releases stress hormones that prepare the body for fight, flight or freeze. The stomach contains many sensory nerves that are stimulated by this chemical surge – hence the “butterflies” we may feel. Fear also causes the vagus nerve to “turn up the volume” on serotonin circuits in the gut. Over-stimulated, the gut goes into high gear and diarrhea can result. People sometimes are “choked with emotion” when the nerves in the esophagus are highly stimulated and trouble swallowing can occur, also resulting in heart burn. Serotonin helps regulate our mood & social behavior, appetite & digestion, sleep, memory, sexual desire and function.
Our central nervous system (CNS) is highly influenced by what we eat. When we feed ourselves, we feed our gut microbiome, which influences everything from our appetite, eating behavior, mood and obesity levels. Our microbiome can also influence our taste, smell, thoughts, impulsivity and compulsivity about food.
Dysfunction in the GBA is common and approximately 60% of women are affected. Symptoms of dysfunction include:
- Fatigue
- Weight gain
- Bloating
- Brain fog
- Anxiety / Anxious
- GI discomfort
- Concentration issues
- Food intolerance or sensitivity
- Impaired memory
An Organics Acid Test (OAT) includes markers for neurotransmitters (serotonin, dopamine, norepinephrine), which can indicate a red flag and problems with the gut-brain-axis.
Many GI disorders like ulcerative colitis and IBS originate from problems with the gut’s brain, and studies have shown it to be involved in Parkinson’s. Up to 90% of our cells are involved in digestive sensations that carry information TO the brain, rather than receiving messages from it. Which means our gut can influence our mood as much as thoughts do.
With our microbiota (aka gut flora), it is key to have a balance of beneficial bacteria for our gut health and mental health. It’s not just the digestion & immune systems that gut microbiota is involved with, but our brain as well. A mix of yeast & bacteria in our intestines can affect messages & chemicals associated with the body’s response to stress, anxiety, and even memory function.
There are anywhere from 10 to 100 trillion microorganism inhabiting our gut – that means there are more microbes in our bowels than in the cells of our body. Our microbiome has more than 1,000 species and 7,000 distinct strains of bacteria. By altering the types of bacteria in our gut, it may be possible to improve our brain health.
If you feel cranky, irritable or depressed, it could be that gut microbiota is out of balance. In the same way, emotions and thoughts can affect how well our body digests food. If the gut is inflamed, bloated or uncomfortable in any way, gut microbiota sends this information the brain – which can directly affect mood.
Here are ways to improve the gut-brain-axis:
- Breath out stress – daily deep breathing cuts the stress & inflammation that disrupt GBA in half. Check out the blogs on Stress for great breathing techniques.
- Steamed vegetables at every meal - they are full of fiber & steaming helps to break down the fiber, making it easier to digest/
- Season with garlic – two cloves a day kills yeast and delivers probiotics to help heal the gut.
Fermented foods - sauerkraut, kimchi, coconut milk yogurt, etc to replenish good bacteria in gut - Drink bone broth - packed with anti-inflammatory amino acids to help heal & seal the gut
- Intermittent fasting – one day each week to reboot the GBA and restore energy – last meal at 7pm and nothing until 9am the next morning.
GBA Foods
- Omega 3 fats – increase good bacterial in gut and reduce risk of brain disorders.
- Fermented foods – healthy microbes shown to alter brain activity (kefir, yogurt, sauerkraut)
- High-fiber foods – contain prebiotic fibers that can reduce stress hormones (whole grains, nuts, seeds, fruits & veggies)
- Polyphenol-rich foods (plant chemicals) increase healthy gut bacteria and may improve cognition (cocoa, green tea, olive oil & coffee)
- Tryptophan-rich foods (amino acid) – converted into neurotransmitter serotonin (turkey, egg, cheese)
Future blogs will talk about how our subconscious mind plays an important role in our health. Studies have shown vast improvement in diseases such as IBS through the use of clinical hypnotherapy.
Until then ~
To Your Health & Happiness,
Michele Root ~ Empowering You!